The information presented in Oncology News Connection (ONC) eNewsletter is provided for physicians and other healthcare providers only and should not be shared with any current or future patients. If you are not a healthcare provider, we welcome you to sign up for Thrive eNewsletter to receive the latest information and blog highlights from Fox Chase Cancer Center.
A relatively new classification of immunotherapeutic drugs is pushing the outer limits of late-line treatment, bringing new hope to patients and the cancer community. They’re bispecific antibodies.
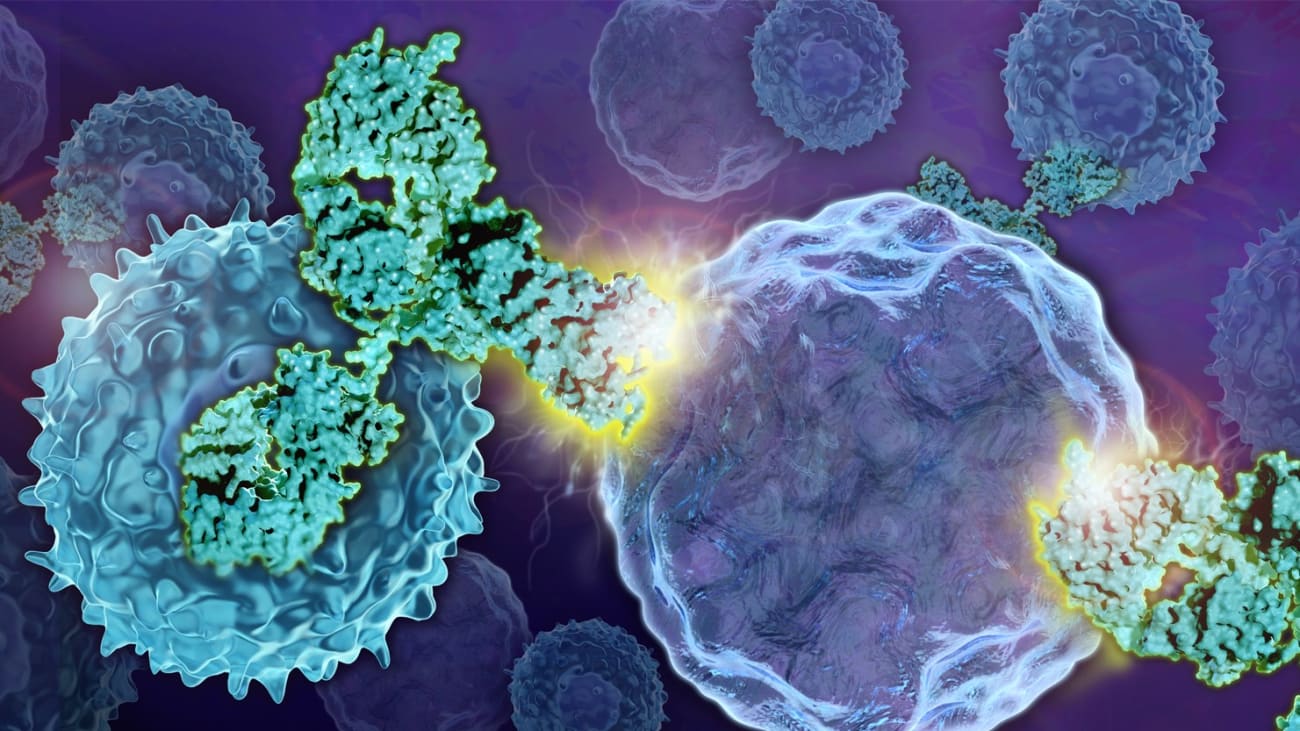
Bispecific antibodies are molecules designed to engage or bind to two different targets, thus capable of bringing two different cells closely together. Most that have gained regulatory approval are T-cell-engaging bispecific antibodies.
For example, the first FDA-approved T-cell-engaging bispecific antibody blinatumomab (Blincyto), approved for patients with acute lymphoblastic leukemia (ALL), binds to CD19 on the surface of B-cell lymphoblasts and to CD3 on the surface of T-cells.
“These drugs label the tumor cells and attract the immune cells to kill the cancer cell,” explained Henry Chi Hang Fung, MD, FACP, FRCPE, chair of the Department of Bone Marrow Transplant and Cellular Therapeutics. “It is like the military’s use of a laser-guided missile. The drug is not only attracting the T-cells but engaging them. That is why it is so powerful.”
Since its initial approval for patients with ALL, several other hematologic malignancies have added a bispecific antibody to the treatment armamentarium.
In October, the FDA approved teclistamab (Tecvayli) for adult patients with relapsed or refractory multiple myeloma who have received at least four prior lines of therapy. Teclistamab binds to B-cell maturation antigen (BCMA), which is expressed on mature B-lymphocytes and plasma cells and CD3. In the trials leading to its regulatory approval, teclistamab elicited responses in more than 60 percent of this heavily treated population.
In December, the FDA granted accelerated approval to bispecific antibody mosunetuzumab-axgb (Lunsumio) for patients with relapsed or refractory follicular lymphoma who have received two or more prior lines of therapy. Mosunetuzumab is a bispecific targeted to CD20—a protein expressed on the surface of B-cells—and CD3. Trials of mosunetuzumab have shown overall response rate of 80 percent, with 60 percent of patients achieving complete disease response.
Another CD20 x CD3 bispecific antibody, glofitamab, is currently under Priority Review with the FDA for treatment of relapsed or refractory diffuse large B-cell lymphoma, with a decision on the drug expected in July.
All of these bispecific antibodies are being used as a late-line treatment option for patients with hematologic malignancies, an area that just recently saw outcome improvements with the approval of another type of immunotherapy, chimeric antigen receptor (CAR) T-cell therapy. All of the currently available CAR T-cell therapies take a patient’s own T-cells, genetically modify them, and re-infuse them into the patient.
“CAR T-cell therapy can be very difficult, and it is almost impossible to imagine it going into frontline treatment because there is too much toxicity,” said Dr. Fung. “Although there are no head-to-head comparisons, [bispecific antibodies] seem as competitive as—if not better than—CAR T-cell therapy, with off-the-shelf availability and the same spectrum of side effects, but with much less toxicity.”
The research pipeline for this drug class holds a lot of promise, with many more bispecific or trispecific antibodies under development.
Researchers at Fox Chase Cancer Center were involved in the MagnetisMM-3 trial, a clinical trial testing another BCMA x CD3-targeting bispecific antibody, elranatamab, in relapsed or refractory multiple myeloma. Results of the trial were presented at the American Society of Hematology 64th Annual Meeting & Exposition in December and showed an impressive objective response rate of 61 percent in patients with no prior BCMA-targeted treatment.
“In the MM-3 study, elranatamab was administered on a weekly schedule, and patients who had an excellent response were allowed to go to an every-two-week schedule after six months,” said Asya Varshavsky-Yanovsky, MD, PhD, Assistant Professor, Department of Bone Marrow Transplant and Cellular Therapies. “The weekly schedule is clearly a burden on the patients. Hopefully, based on the results of the MM9 study, the dosing schedule can be changed and patients will be able to enjoy fewer interruptions to their normal lifestyle.”
Bispecific antibodies are also gaining traction in the treatment of certain solid tumors.
The FDA has approved tebentafusp-tebn (Kimmtrak) for HLA-A*02:01-positive adult patients with unresectable or metastatic uveal melanoma. Also a bispecific T-cell engager, tebentafusp binds to gp100 peptide-HLA and CD3.
Hossein Borghaei, DO, MS, Chief of the Division of Thoracic Medical Oncology at Fox Chase, presented results of a phase-1 trial of another bispecific T-cell engager, tarlatamab, in the treatment of small cell lung cancer (SCLC) at the 2022 World Conference on Lung Cancer. Tarlatamab binds to DLL3, which is overexpressed in most SCLC and CD3. These early results showed an overall response rate of 24 percent in patients with pretreated SCLC. Among patients who experienced disease response, the median duration of response was longer than one year.
“Bispecific antibodies and bispecific T-cell engagers are exciting and innovative drugs that could impact patient care in the future,” Dr. Borghaei said. “Drugs like tarlatamab, if successful and approved, could provide new treatment options for patients with solid tumors like small cell lung cancer.”